At Khandwala Eye Hospital You will be cared by an excellent Ophthalmologists for both your preoperative and postoperative visits. Here, Laser Vision Correction includes a pre-procedure visit and a thorough examination, the procedure itself, and all follow-up care to ensure the best possible results.
Understanding Retina of an Eye
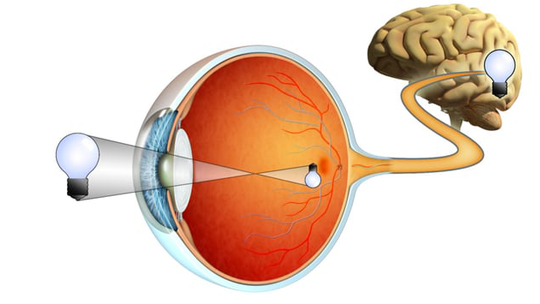
How the Retina Allows Us To See..
The retina is the light-sensitive tissue lining the back of our eye. Light rays are focused onto the retina through our cornea, pupil and lens. The retina converts the light rays into electrical impulses that travel through the optic nerve to our brain, where they are interpreted as the images we see. A healthy, intact retina is needed for clear vision. It functions like the film in a camera, capturing images focused by the structures in the front of the eye. After capturing the images, it transmits them to the brain. The macula is a small area at the center of the retina that gives us our pinpoint central vision. The area of retina surrounding the macula gives us our peripheral vision.
Our Retina Specialists are equipped to treat all kinds of the medical and surgical diseases affecting the vitreous, macula, and retina of patients of all ages.
Retinal Cell Imaging.
We employ the most computerised advanced tools in the diagnosis ( Fundus fluorescein angiography, Ultrasound B Scan, OCT & Visual Electrophysiological Tests such as ERG, multifocal ERG, VEP and EOG ) of diseases of the retina.
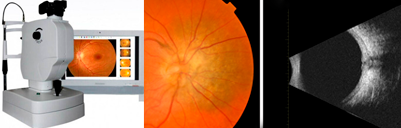
An overview of OCT machine..
A Fundus fluorescein angiography helps us in recording using a confocal scanning laser ophthalmoscope (cSLO) in place of the conventional fundus camera. This complex instrument uses a laser beam of the appropriate excitation wavelength to scan across the fundus in a raster pattern to illuminate successive elements of the retina, point-by-point. This test is often used by us to manage eye disorders.Human Eye - Structure and Function.
The Retina Translates Light to Meaning..
The eye is a marvelous organ that takes light and, in partnership with the nervous system, transforms it into a meaningful scene. It’s also very self-sufficient. It is self-focusing, self-adjusting, and self-cleaning. The job of focusing incoming light is occupied by the retina, which works closely with the brain, to allow us to see the faces of our loved one, beautiful vistas, and the pages of a good book.The retina performs an enormous task. Not only is it translating light into meaning, it is acting as editor and curating, sifting out information and only processing what is useful for the viewer. The rest of the eye works diligently to focus the light rays that eventually make it to the retina.

Some of the Retinal conditions treated at K.E.H
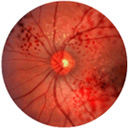
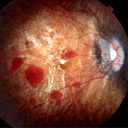
Diabetic Retinopathy.

Chronically high blood sugar from diabetes is associated with damage to the tiny blood vessels in the retina, leading to diabetic retinopathy. The retina detects light and converts it to signals sent through the optic nerve to the brain. Diabetic retinopathy can cause blood vessels in the retina to leak fluid or hemorrhage (bleed), distorting vision. In its most advanced stage, new abnormal blood vessels proliferate (increase in number) on the surface of the retina, which can lead to scarring and cell loss in the retina.
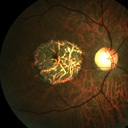
Age-Related Macular Degeneration.
 Age-related macular degeneration (AMD) is a deterioration or breakdown of the eye's macula. The macula is a small area in the retina — the light-sensitive tissue lining the back of the eye. The macula is the part of the retina that is responsible for your central vision, allowing you to see fine details clearly.Many people are not aware that they have macular degeneration until they have a noticeable vision problem or until it is detected during an eye examination.
Age-related macular degeneration (AMD) is a deterioration or breakdown of the eye's macula. The macula is a small area in the retina — the light-sensitive tissue lining the back of the eye. The macula is the part of the retina that is responsible for your central vision, allowing you to see fine details clearly.Many people are not aware that they have macular degeneration until they have a noticeable vision problem or until it is detected during an eye examination.
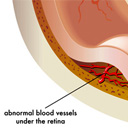
Retinal Detachment.
 Retinal detachment describes an emergency situation in which a thin layer of tissue (the retina) at the back of the eye pulls away from its normal position.Retinal detachment separates the retinal cells from the layer of blood vessels that provides oxygen and nourishment. The longer retinal detachment goes untreated, the greater your risk of permanent vision loss in the affected eye. Warning signs of retinal detachment include the sudden appearance of floaters and flashes and reduced vision. Contacting an eye specialist (ophthalmologist) right away can help save your vision.
Retinal detachment describes an emergency situation in which a thin layer of tissue (the retina) at the back of the eye pulls away from its normal position.Retinal detachment separates the retinal cells from the layer of blood vessels that provides oxygen and nourishment. The longer retinal detachment goes untreated, the greater your risk of permanent vision loss in the affected eye. Warning signs of retinal detachment include the sudden appearance of floaters and flashes and reduced vision. Contacting an eye specialist (ophthalmologist) right away can help save your vision.
Macular Hole.
 A macular hole is a small break in the macula, located in the center of the eye's light-sensitive tissue called the retina. The macula provides the sharp, central vision we need for reading, driving, and seeing fine detail. A macular hole can cause blurred and distorted central vision. Macular holes are related to aging and usually occur in people over age 60.The size of the hole and its location on the retina determine how much it will affect a person’s vision. When a Stage III macular hole develops, most central and detailed vision can be lost. If left untreated, a macular hole can lead to a detached retina, a sight-threatening condition that should receive immediate medical attention.
A macular hole is a small break in the macula, located in the center of the eye's light-sensitive tissue called the retina. The macula provides the sharp, central vision we need for reading, driving, and seeing fine detail. A macular hole can cause blurred and distorted central vision. Macular holes are related to aging and usually occur in people over age 60.The size of the hole and its location on the retina determine how much it will affect a person’s vision. When a Stage III macular hole develops, most central and detailed vision can be lost. If left untreated, a macular hole can lead to a detached retina, a sight-threatening condition that should receive immediate medical attention.
Epiretinal Membrane.
 An epiretinal membrane is a thin sheet of fibrous tissue that can develop on the surface of the macular area of the retina and cause a disturbance in the vision. An epiretinal membrane is also sometimes called a macular pucker, premacular fibrosis, surface wrinkling retinopathy or cellophane maculopathy. Most epiretinal membranes happen because the vitreous (the jelly inside the eye) pulls away from the retina. This most commonly happens to people over the age of 50. The membrane may also form following eye surgery or inflammation inside the eye.
An epiretinal membrane is a thin sheet of fibrous tissue that can develop on the surface of the macular area of the retina and cause a disturbance in the vision. An epiretinal membrane is also sometimes called a macular pucker, premacular fibrosis, surface wrinkling retinopathy or cellophane maculopathy. Most epiretinal membranes happen because the vitreous (the jelly inside the eye) pulls away from the retina. This most commonly happens to people over the age of 50. The membrane may also form following eye surgery or inflammation inside the eye.
Myopia Maculopathy.
 Eyes which have short sightedness of over 600 degrees are classified as having high myopia. Myopia occurs when the eyeball is too long and light rays entering the eye are unable to focus on the light-sensitive part of the eye called the retina. In high myopia, the excessive elongation of the eyeball leads to degeneration of the retina, in particular, to a central part of the retina called the macula. The macula has the highest concentration of cones (light sensitive cells that interpret colour images) in the retina and plays a central role in processing detailed images.
Eyes which have short sightedness of over 600 degrees are classified as having high myopia. Myopia occurs when the eyeball is too long and light rays entering the eye are unable to focus on the light-sensitive part of the eye called the retina. In high myopia, the excessive elongation of the eyeball leads to degeneration of the retina, in particular, to a central part of the retina called the macula. The macula has the highest concentration of cones (light sensitive cells that interpret colour images) in the retina and plays a central role in processing detailed images.
Serous Chorioretinopathy.
 In central serous retinopathy (sometimes called central serous choroidopathy), fluid builds up under the retina and distorts vision. Fluid leakage is believed to come from a tissue layer with blood vessels under the retina, called the choroid. Another layer of cells called the retinal pigment epithelium (RPE) is responsible for preventing fluid from leaking from the choroid under the retina. When, for unknown reasons, tiny areas of the RPE become defective, fluid builds up and accumulates under the RPE, much as liquid in a blister collects under the skin. As a result, a small detachment forms under the retina, causing vision to become distorted. Central serous choroidopathy usually affects just one eye at a time, but it is possible that both eyes may be affected at the same time.
In central serous retinopathy (sometimes called central serous choroidopathy), fluid builds up under the retina and distorts vision. Fluid leakage is believed to come from a tissue layer with blood vessels under the retina, called the choroid. Another layer of cells called the retinal pigment epithelium (RPE) is responsible for preventing fluid from leaking from the choroid under the retina. When, for unknown reasons, tiny areas of the RPE become defective, fluid builds up and accumulates under the RPE, much as liquid in a blister collects under the skin. As a result, a small detachment forms under the retina, causing vision to become distorted. Central serous choroidopathy usually affects just one eye at a time, but it is possible that both eyes may be affected at the same time.
Retinal Vascular Disorders.
 Retinal vascular disorders refer to a range of eye diseases that affect the blood vessels in the eye. If you are experiencing blurred vision, you may be having retinal vascular disorders. Retinal vascular diseases can be triggered by medical conditions such as high blood pressure, cardiovascular disorders, diabetes, bleeding, clotting, autoimmune disorders, history of stroke, and artherosclerosis or the thickening of blood vessels. Other factors such as age, high cholesterol, using oral contraceptives, being overweight and smoking can also add up to a person’s likelihood of developing retinal vascular disorders.
Retinal vascular disorders refer to a range of eye diseases that affect the blood vessels in the eye. If you are experiencing blurred vision, you may be having retinal vascular disorders. Retinal vascular diseases can be triggered by medical conditions such as high blood pressure, cardiovascular disorders, diabetes, bleeding, clotting, autoimmune disorders, history of stroke, and artherosclerosis or the thickening of blood vessels. Other factors such as age, high cholesterol, using oral contraceptives, being overweight and smoking can also add up to a person’s likelihood of developing retinal vascular disorders.
Floaters & Flashes.
 Floaters look like small specks moving in front of your eyes. They are actually tiny clumps floating through the clear gel in your eye.Flashes look like lightening streaks. They happen when the gel pulls on its attachment to your retina, the part of the eye that senses light.Floaters and flashes may mean there is a problem with your retina, the layer of nerve tissue at the back of the eye. A torn retina is serious.Floaters may appear as different shapes, such as specks, clouds, dots, circles, lines, or cobwebs. You can often see them when looking at a plain background, like a blank wall or blue sky. Clumps and strands within the gel of the eye cast shadows on the retina, the layer of cells lining the back of the eye that senses light and allows you to see. Flashes look like flashing lights or lightning streaks. They can appear off and on for several weeks, and become more common with age. Some people experience flashes of light that appear as jagged lines or “heat waves” in both eyes at once, lasting 10 to 20 minutes. These types of flashes are usually caused by a spasm of blood vessels in the brain, which is called migraine.If you suddenly notice an increase in floaters or flashes, see your ophthalmologist (Eye M.D.) right away.
Floaters look like small specks moving in front of your eyes. They are actually tiny clumps floating through the clear gel in your eye.Flashes look like lightening streaks. They happen when the gel pulls on its attachment to your retina, the part of the eye that senses light.Floaters and flashes may mean there is a problem with your retina, the layer of nerve tissue at the back of the eye. A torn retina is serious.Floaters may appear as different shapes, such as specks, clouds, dots, circles, lines, or cobwebs. You can often see them when looking at a plain background, like a blank wall or blue sky. Clumps and strands within the gel of the eye cast shadows on the retina, the layer of cells lining the back of the eye that senses light and allows you to see. Flashes look like flashing lights or lightning streaks. They can appear off and on for several weeks, and become more common with age. Some people experience flashes of light that appear as jagged lines or “heat waves” in both eyes at once, lasting 10 to 20 minutes. These types of flashes are usually caused by a spasm of blood vessels in the brain, which is called migraine.If you suddenly notice an increase in floaters or flashes, see your ophthalmologist (Eye M.D.) right away.
Proliferative Vitreoretinopathy.
 Proliferative Vitreoretinopathy (PVR) occurs when a scar forms under or on the retina after retinal detachment, preventing the retina from healing and falling back into place. When there is a hole in the retina, cells that normally reside under the retina enter the eyeball and settle on the inner layer of the eye on top of the retina. These cells multiply and form a scar on the surface (and sometimes under) the retina. This scar tissue then contracts and detaches the retina away from the innermost walls of the eye, resulting in a second retinal detachment.Proliferative vitreoretinopathy (PVR) may be treated with a vitrectomy, a form of keyhole surgery that uses small probes to enter inside the eye to remove the vitreous and or scleral buckling, an operation using a silicone bane outside the eyeball. If vitrectomy is performed, gas or silicone oil may be used to replace the jelly inside the eye. Following surgery, the patient will need to lie in a face-down position for one to two weeks. Eyes with serious PVR may not be treated with surgery if the vision is unlikely to improve after surgery. The success of improving the vision varies from person to person and ranges from 60 to 80 per cent.
Proliferative Vitreoretinopathy (PVR) occurs when a scar forms under or on the retina after retinal detachment, preventing the retina from healing and falling back into place. When there is a hole in the retina, cells that normally reside under the retina enter the eyeball and settle on the inner layer of the eye on top of the retina. These cells multiply and form a scar on the surface (and sometimes under) the retina. This scar tissue then contracts and detaches the retina away from the innermost walls of the eye, resulting in a second retinal detachment.Proliferative vitreoretinopathy (PVR) may be treated with a vitrectomy, a form of keyhole surgery that uses small probes to enter inside the eye to remove the vitreous and or scleral buckling, an operation using a silicone bane outside the eyeball. If vitrectomy is performed, gas or silicone oil may be used to replace the jelly inside the eye. Following surgery, the patient will need to lie in a face-down position for one to two weeks. Eyes with serious PVR may not be treated with surgery if the vision is unlikely to improve after surgery. The success of improving the vision varies from person to person and ranges from 60 to 80 per cent.
Lattice Degeneration.
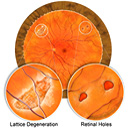 Lattice degeneration complicated by tractional tears as the result of an acute, symptomatic posterior vitreous detachment represents a high-risk situation for future retinal detachment and is an urgent indication for laser retinopexy. Although multiple theories have been suggested about the cause of this disease, the factors which lead to lattice eye degeneration remain largely unknown. Diseased eyes may have vascular deficiencies, meaning the network of vessels which supplies blood to the retina is underdeveloped. A hereditary element is suspected as well.Lattice degeneration is a relatively common condition causing areas of peripheral retinal thinning. Although usually not progressive, lattice may lead to retinal detachment and temporary or permanent loss of vision
Lattice degeneration complicated by tractional tears as the result of an acute, symptomatic posterior vitreous detachment represents a high-risk situation for future retinal detachment and is an urgent indication for laser retinopexy. Although multiple theories have been suggested about the cause of this disease, the factors which lead to lattice eye degeneration remain largely unknown. Diseased eyes may have vascular deficiencies, meaning the network of vessels which supplies blood to the retina is underdeveloped. A hereditary element is suspected as well.Lattice degeneration is a relatively common condition causing areas of peripheral retinal thinning. Although usually not progressive, lattice may lead to retinal detachment and temporary or permanent loss of vision
Retinal Tears.
 A retinal tear occurs when part of the retina separates from the outer layers of the eye. If not treated early, retinal tears can lead to a more serious condition called retinal detachment, which may lead to partial or complete loss of vision.Retinal tears occur when the gel-like vitreous in the eye becomes more liquid and exerts an abnormal pull on the retina. Retinal tears are painless. Some symptoms include seeing an increased number of floaters and flashes, and decreased vision. Floaters are small, moving spots in the field of view and can even be seen when the eyes are closed. A sudden increase in number or size of floaters may suggest a retinal tear. Flashes, the seeing of a bright light in your field of vision, is also a possible sign of a retinal tear. This happens when the vitreous pulls on the retina and causes a bright visual response. Retinal tears can progress to a more serious stage when retinal detachments occur, so early detection of retinal tears are essential to prevent the problem from worsening.Retinal tears are usually treated with laser treatment to prevent the retinal tear from developing into retinal detachment. Laser treatment works by forming a scar around the retinal tear and prevents the vitreous from seeping through the tear. Some retinal tears need not be treated as they may not lead to retinal detachment. However they may still need to be observed and followed up to ensure that the retina remains stable. Treatment of retinal tear is usually successful with a success rate of 95 per cent and early treatment of retinal tear can preserve normal vision and prevent severe vision loss.
A retinal tear occurs when part of the retina separates from the outer layers of the eye. If not treated early, retinal tears can lead to a more serious condition called retinal detachment, which may lead to partial or complete loss of vision.Retinal tears occur when the gel-like vitreous in the eye becomes more liquid and exerts an abnormal pull on the retina. Retinal tears are painless. Some symptoms include seeing an increased number of floaters and flashes, and decreased vision. Floaters are small, moving spots in the field of view and can even be seen when the eyes are closed. A sudden increase in number or size of floaters may suggest a retinal tear. Flashes, the seeing of a bright light in your field of vision, is also a possible sign of a retinal tear. This happens when the vitreous pulls on the retina and causes a bright visual response. Retinal tears can progress to a more serious stage when retinal detachments occur, so early detection of retinal tears are essential to prevent the problem from worsening.Retinal tears are usually treated with laser treatment to prevent the retinal tear from developing into retinal detachment. Laser treatment works by forming a scar around the retinal tear and prevents the vitreous from seeping through the tear. Some retinal tears need not be treated as they may not lead to retinal detachment. However they may still need to be observed and followed up to ensure that the retina remains stable. Treatment of retinal tear is usually successful with a success rate of 95 per cent and early treatment of retinal tear can preserve normal vision and prevent severe vision loss.
Hereditary Macular Dystrophies.
 Hereditary macular dystrophies are degenerative diseases of the central area of the retina associating primary anomalies of the retinal pigment epithelium and sensory retina. These conditions, whose hallmark is a loss of visual acuity, are a major cause of blindness and affect patients at all ages. Macular dystrophies group diseases that are heterogenous at the genetic level, as well as at the clinical, histological and physiopathological levels. Monogenic macular dystrophies are rare autosomal dominant conditions, with the exception of Stargardt disease in its typical form, which is not only relatively frequent but is also inherited as an autosomal recessive trait. Several mutations in separate genes have been linked to these disorders suggesting that this group is genetically as well as clinically heterogeneous.
Hereditary macular dystrophies are degenerative diseases of the central area of the retina associating primary anomalies of the retinal pigment epithelium and sensory retina. These conditions, whose hallmark is a loss of visual acuity, are a major cause of blindness and affect patients at all ages. Macular dystrophies group diseases that are heterogenous at the genetic level, as well as at the clinical, histological and physiopathological levels. Monogenic macular dystrophies are rare autosomal dominant conditions, with the exception of Stargardt disease in its typical form, which is not only relatively frequent but is also inherited as an autosomal recessive trait. Several mutations in separate genes have been linked to these disorders suggesting that this group is genetically as well as clinically heterogeneous.